‘C’ IN CANCER IS ALSO FOR COURAGE, COMPASSION & CARE
This month on the blog we have Mugdha Rahatekar, giving a first-hand account of her tryst with cancer and what it entails. Today, marks one year since her diagnosis. In her own honest and heartfelt words she writes positively about sailing through with courage.
You Never Know
Boy, what a year it’s been!
Last year during May, Pravin (my husband) and I took our annual vacation; San Francisco (SFO) this time to celebrate 16 years of togetherness. One of our best trips by far with a lovely weather, beautiful landscapes and catching up with family and friends; couldn’t have gone any better! But you never know what’s waiting for you just around the corner.
A week after our return, on a Friday evening, after leaving work I felt discomfort in my stomach / abdomen. Came home, wasn’t able to pee (I usually drink a lot of water so it felt like my bladder was going to burst), so went to an Urgent Care where they thought it’s a case of UTI (Urinary Tract Infection), gave me meds and sent me back home. I called one of my best friends, a confidante and a doctor and she suggested that I go to the ER, since it would be some time before the medication took effect (and that was one of the best decisions I took that night). The ER visit was followed by a rapid succession of blood tests and a CT scan. I had a mass on the left ovary. We were in the ER from 8:30 pm to 5:00 am the next day, where they had to also put in a catheter. For 12 hours I hadn’t been able to pass urine and it was probably the worst night of my life!
I was referred to a gynaecologist and urologist. My Primary Care Physician scheduled an appointment for me to see a gynaecologist oncologist (gyn-oncologist) and we met him on 6th June (I still had the catheter in me). He speculated the mass might be a fibroid and recommended an ultrasound. We were on our way back from the hospital when he called to say that the mass looked suspicious and would require a surgery at the earliest.
When we went to see the gyn-oncologist for my pre-op appointment for the surgery on 11th June he told us that the mass wasn’t a fibroid or a cyst but a tumour, which may or may not be malignant. He explained that it would be an open incision surgery, and involve removal of the tumour, the left ovary, and the fallopian tube. He further explained that if anything suspicious was found, we should be prepared for a full hysterectomy (removal of the ovaries, uterus, fallopian tubes, and omentum). We signed the consent form. A freeze histopathology during the surgery did not suggest malignancy, so a full hysterectomy did not happen and I was home in a couple of days.
With an open incision surgery the healing is prolonged. In the second week post-surgery (on 19th June), the gyn-oncologist called to enquire about my recovery and then conveyed that the biopsy results showed a cancerous tumour. Also, due to endometriosis, the tumour had been stuck and it had ruptured during the excision. The doctor advised a second surgery, 6 weeks after my first one, to have a radical hysterectomy. It was something none of us had expected.
After a few follow-up appointments I was back at the hospital on 22nd July for the second surgery. It was a laparoscopic procedure, took 5.45 hours (due to the endometriosis and scar tissue from the previous surgery), and I had a radical hysterectomy. Chemotherapy was recommended, irrespective of the biopsy results of the second surgery. A bit of good news (finally!) came in a week later; the cancer hadn’t spread to any organs taken out or to any lymph nodes. It was stage 1C ovarian cancer (if the tumour hadn’t burst it might have even been classified as stage 1A).

Mugdha, happy & healthy. Before her diagnosis.
Cancer In, Cancer Out
I am not sure how cancer gets in. How does it start? I had no symptoms before that first visit to the ER. A lot happens once it’s in your body though. Medically, it involves doctor visits, surgery, chemotherapy and endless trying-to-gain-knowledge sessions. Here are a few “medical” things that I learned over the past few months. There is a marker test that checks the “CA-125” level for ovarian cancer; the normal range is below 35 and mine was 125 when I started having trouble. A high number on the CA-125 might be due to other reasons, but since there is no other test (no, pap smear does not help detect ovarian cancer, it helps detect uterine cancer) to help detect ovarian cancer it doesn’t hurt to have your gynaecologist get this in with the routine blood work.
Next step was to begin chemotherapy. The gyn-oncologist suggested I get a port, so that I would not have to be poked and prodded each time. I would require either 4 or 6 sessions. Everybody has a different reaction or effect to the chemotherapy drugs. My gyn-oncologist stopped one of the medications after 4 sessions since it caused tingling and numbing and they did not want it to become permanent. Anyone undergoing chemotherapy should make sure their oncologist is aware of any side effects felt and weigh-in on whether the effects are worth the treatment or not. I was lucky to have a good PCP and gyn-oncologist and did not need a second opinion. If you are not sure about the diagnosis your doctor has given, make sure you voice your concerns and / or get a second opinion. Remember, if you don’t speak up, it might affect your health. Going from feeling healthy to taking time to recover is no fun! I had a total of 6 chemotherapy sessions with my last session being on 31st December 2019; I was glad to be able to start 2020 cancer-free, treatment-free. On 2nd June 2020, I got the 6 month follow-up and CT scan results and I have been told everything looks good. They say ovarian cancer is a silent killer. In about 85% cases, it isn’t detected until it’s too late; I was fortunate to be in the other 15%!
Being Practical
My parents had rushed down from India within 4 days to be with us. We had huddled around with the phone on speaker when the doctor had first called to disclose the reports. They were beside themselves on hearing ‘malignant’. I remember trying to be practical- for them and for me. I couldn’t falter, I felt the need to be strong for my family. For once accepting that cancer can happen to me too. Acceptance helps, in more ways than you can think.
I resumed work post-surgery and continued working throughout the chemotherapy. 2 weeks into chemotherapy my husband shaved my head for good. My scalp had started to feel tender (it hurt even when I put my head on the pillow) and every time I ran my fingers through my hair I saw a few hair come out. Will it be just thinning or is it time to shave my head (as planned) were some of the thoughts running through the mind. Over the next few days, I started seeing hair strands on pillows and clothes, so shaving my head was the next practical step for me. I went for a look which I haven’t had since I was a baby probably, then too I don’t think I was bald.

Smiling through the side-effects of chemotherapy.
Coping Mechanisms
‘Problems are not the problem; coping is the problem”.
Let’s be clear here- you cannot minimize or tolerate stress and conflict by yourself. As someone who has faced this, I would say, you get there little at a time- accepting, hoping, and being courageous. No matter the problem, one has to find his/her own way of coping. Retrospectively, I could cope because I had a strong support system.
An ex-colleague, who had undergone chemotherapy, had prepped me on what to expect during the sessions. He had said that more than pain what gets you is exhaustion and I understood that once I started going through it. Since chemotherapy kills goods cells along with the bad ones, your energy levels go down, you feel mostly tired, and there are several other effects of the drugs; it depends on what drugs are used for the treatment and also on how your body responds. My worst symptoms and effects from the drugs were nausea, feeling exhausted quickly, not being able to eat a lot of foods (mostly because the smell made me nauseous), getting a numbing / tingling sensation in my fingers and hands and toes and feet, scalp pain, and hair loss. Others whom I know have experienced other effects like weight loss due to loss of appetite, vomiting, and hair loss.
It was comforting to have my parents with us; to see them unwavering when I shaved my head and when I struggled with chemotherapy symptoms. My in-laws, who could not come to the US, were equally devastated to hear about my diagnosis and kept praying and checking up on me. Our nephew who lives with us took responsibility of the kitchen, once my parents flew back, since I was still nauseous and couldn’t cook. Family members kept a check through parents and cousins; my cousins have been a big support system. Some of my close friends here made sure we had everything we needed and offered to help out in any way. How can I not mention Pravin, without whom I would not have been able to do anything! Having his shoulder to lean on and his hand to hold helped tremendously; it isn’t easy to go through anything alone.
You always have someone in your life like that, all you need to do is take the second step and ask for help if you need it. Don’t be shy or feel that asking for help is cowardly.
Working throughout the chemotherapy phase helped me physically and mentally; like bringing a sense of normalcy. It was wonderful to have an extended family at work. They have been there throughout, being accommodating knowing that I would not be able to work full time during and a few months after the treatment; I have to mention my boss, who has been very understanding and given me the time and space I needed while recovering. A dearest friend’s mom (at the workplace), a cancer survivor herself, sent me a lovely cap that she knit knowing that my head would get cold once the chemotherapy started. She still checks on me every now and then.
I want to thank my doctors and nurses who helped me understand what I was going through, made the right decisions in regards to my health, and answered all my questions every step of the way, patiently.
A friend sent me a care basket that included a lot of “yellow” things to bring me sunshine; among that was a colouring book and I took up pencil colouring and colouring on my tablet, a nice distraction which helped me stay relaxed. For a talkative person like me doing video calls with family and friends brought lot of happiness (very rarely do we grab a chance to catch-up in our busy lives). I got caught up on some comedy movies and TV shows that I had added to my watch list but never had the time before. Once I was well enough to go out, we started going out on weekends, a very important thing for an outdoor person like me! I had also missed driving during the recovery period and once my doctor cleared me medically, I started driving and taking my parents out for some time and that helped me feel like I was getting back to my normal self. Every kind gesture, every comforting call, and every thoughtful action just made it that much easier to sail through it all.
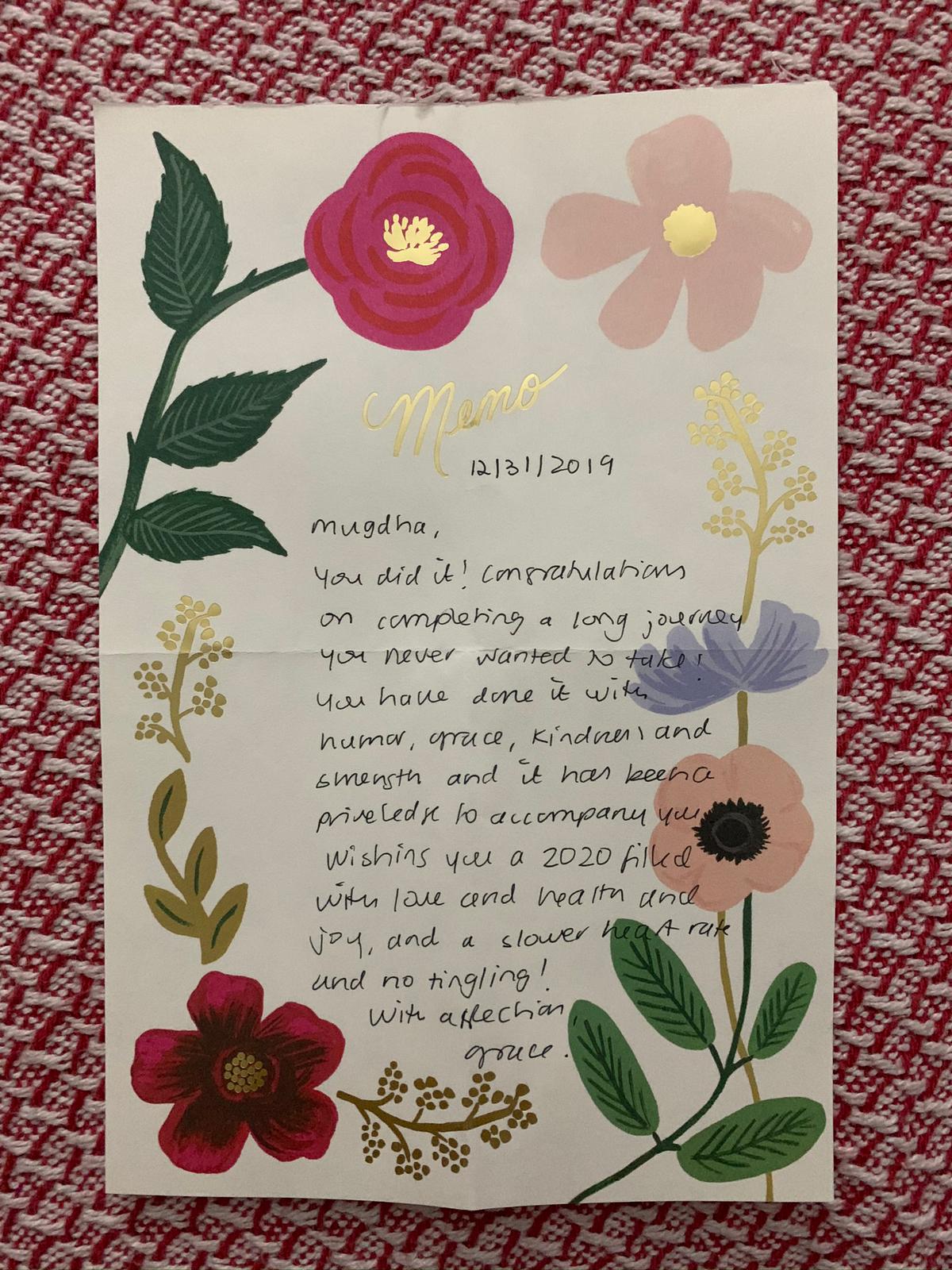
Gifted by the oncology nurse on the last day of Mugdha’s chemotherapy session.
Learning Curve
Through all this, I learned a lot about myself. I am stronger than I thought I was. I never thought I would go through something like this (no one does!). What kept me strong, sane and ready to face the challenges were the people who love and care for me, practicing what I preach-what’s going to happen will happen, if we accept it and face it willingly, it becomes a little less difficult to go through, being positive and being happy. Hearing that you have cancer is a lot to handle, going through it is a lot more!
Though cancer is widely known, I think we are more ready than before to actually talk and listen about it. What needs to stop is the stigma around it. Different people react differently to news of cancer. Some were not sure about what to ask or say to me, and they stopped contacting me. May be they thought I might not be in the best of my mental health to talk to them, assumed that I was / might be depressed and did not feel comfortable talking to me. I have nothing against them; but I never had a problem talking about what I was going through. There were some who distanced from us after my diagnosis, there were others (who I hadn’t been in touch with for a long time) who heard about me through common friends or relatives and reached out to me to ask about my health and tell me that things were going to be fine; that I was a strong person who they looked up to. That they took the first step made a huge difference to me!
Something a friend once said to me has stuck with me. She said, “You are in the USA, so you can shave your head without thinking about what people will say. It’s not easy doing that in India; people stare at you and look at you like your “baldness” is contagious”. I wouldn’t bother much about what each and every person says or thinks unless they are close to me and I value their opinion. So my natural thought was, that shouldn’t matter; but in reality, if I were in a place where I would experience such reactions from people, would I have done it so easily? I am not 100% sure.

Mugdha post-recovery. That smile reflects the lovely, strong and perpetually transformed inner strength.
There’s always something in everyone’s life worth living for, it might take longer for some to figure out what it is.
Get to know / learn as much as possible about the situation or problem you are facing and try to find a solution. It may not always be easy, or the right one; but you won’t know till you try.
This blog is about little Ira's journey through cancer and dealing with it together as a family. It is also about building a perspective of life, spreading things worth sharing and of love and hope.
Beautiful Journey and I salute you for your positivity and courage
Thank you so much Bhushan bhai!
I salute your positive nature and courage Be happy for ever I pray for long life.
Thank you so much Lata aatya!
Well fought sis👏🏻👏🏻 Your courage positivity n determination worked like a magic potion!!! Of course your super strength Pravin, always by your side n the love n blessings of your parents all blended in!! You Won!!! Shine on girl🌟
❤️ Always
Thank you my dear sis 😘
You are a very courageous girl and you have really gone through it and successfully overcome it. I really appreciate your will power to face such a challenge. I know you were very well supported by Pravin, Your Parents, Your Nephew, Your Inlaws and your Friends. Improve upon your health and we wish you a very happy and healthy life. In case you require any support kindly communicate and we will do it for you.
Thank you so much kaka kaku!
Mugdha,
Reading and knowing your journey that close has been an eye opening and heart warming thing at the same time.
We often just say and preach that positivity, smile, courage, and faith are the things that are needed to sail through this journey Called life but you have lived it and proved it Yet again 👍
It’s so difficult to smile in tough times but you always did it and you never showed any of your dull, depressing moments to the world ( which I am sure you must have had ) .. kudos for that 🙏
You have been an inspiration for sure and I wish you amazing health and happening life ahead 😊😊
Thank you Siddha 🙂
Mugdha, I admire your courage and positive view towards the life . Take care & always keep smiling my dear friend…
Thanks so much Archu!
Penned down wonderfully. Even though you have mentioned a lot. I am sure there are a lot more unsaid emotions and things.
I know you are brave and have come out of the dark tunnel beautifully.
It’s extremely hard to walk this path.
Love you loads…
Keep smiling…
Prads
Thanks so much Prads! Who would know it better than you? You’re one of my inspirations ❤️
Dear, sweet Mugs thank you for sharing this journal of your journey fighting and overcoming cancer. Although we’ve chatted throughout this trial, reading and rereading your words has given me a deeper insight into your heart, determination and loving husband, Pravin, along with your parents, in-laws and numerous friends who have supported and loved you throughout this journey.
You, my dear friend, kicked cancer in the buttocks and conquered the beast. I’m so proud of your courage and determination and am honored to have you as my dear friend.
Always in my thoughts and prayers,
Dawn
Thank you so much Mama Dawn! You should know that you’re one of those who was there to listen to me throughout this 🤗 and I sincerely appreciate that!
Vahini you are extremely strong and your positive view towards the life absolute inspiration… Keep smiling
Thank you so much Milind
BRAVE..u shall inspire millions…good to have u back..take care..
Thank you Deven!
Congratulations on your recovery. Inspirational journey..
Thank you Deepali
Fantastic courage shown and maturity with which you have faced it…bravo….
Thank you so much Balu mama!
Brave girl. Your thoughts will definitely inspire others as how to face the difficult situation. Stay healthy and continue to spread happiness to others as usual.
Thank you so much kaka!
Mugdha you are real fighter… being positive is most important and you ensure through out your journey. I also want highlight Praveen’s role was very important and it is also very important to have emotional connection always… Praveen hats off buddy…
So happy to see refreshed Mugdha back…
Thanks so much Rahul!
You are so brave. Your fight is inspiring and hope for others.
Thanks so much DJ!
Mugdha, you are light of joy!! Grateful that you choose to share your struggle and your victory. Your wisdom will help many as it helps us all see life in a beautiful positive light.
We adore you! Keep smiling 💞
Thank you so much Hemangi 🤗
Congratulations on your fast recovery. Hope you are doing well, keep up the big smile, it is inspiring!
Thank you so much Touhami! You reading this means a lot to me 😊.
Mugdha hats off to you and we hope you will enjoy the life to the fullest extent. Hope you, with your hubby will visit India as early as possible.
Thank you so much aai baba. ❤️ Love you both so much ❤️
Thanks for sharing your strong journey, Mugdha. You are an inspiration to others who might be facing similar challenges. Wish you a long and fulfilling life!
Thank you so much Meeta! 🤗
Hi Mugdha,
Bravo! First, let me congratulate you for your victory over Cancer and brave fight against this. I know that you are a positive person and your positivity must have gone up in multiples when a person like Pravin is with you to care.
I am glad that you have recovered well and are doing fine and I wish you The best in life. Take care and keep smiling,,,😊
Thanks so much Atul! 🤗
Hi Mugs, what a courageous pragmatic approach you kept in your fight for cancer ♋ as well as penning it down. 👏
Telepathy works, last Valentine’s day to counter negativity of Covid, I mentioned in detail about your and your parents as epitome of positivity.
Take care my dear ❤😘
Lots of love 💕 and hugs 🤗
Raks4u
Thank you so much Raks!